Fertility.
Fertility refers to the ability to conceive a pregnancy. Around 1 in 6 couples experience difficulties conceiving, and this can be an emotional and overwhelming journey. The good news is that many causes of subfertility are treatable, and early assessment offers the best chance of success.
What Is Infertility?
Infertility is defined as:
Not achieving pregnancy after 12 months of regular unprotected intercourse (or 6 months if the woman is over 35 years).
It may be female-factor, male-factor, or a combination, and in some cases no clear cause is found (unexplained infertility).
Causes of Infertility
Female Factors
Ovulation problems (eg. polycystic ovary syndrome, thyroid disorders)
Endometriosis
Tubal blockage or damage (eg. previous pelvic infection, surgery, adhesions)
Fibroids, particularly those affecting the uterine cavity
Low ovarian reserve or age-related egg decline
Uterine abnormalities such as polyps, septum, or scarring
Male Factors
Low sperm count
Poor sperm motility (movement)
Abnormal sperm shape
Blockages in the reproductive tract
Lifestyle factors (smoking, heat exposure, excessive alcohol, certain medications)
Combined or Unexplained
In around 20–30% of couples, both partners have contributing factors.
Unexplained infertility is diagnosed when all investigations are normal but pregnancy is still not achieved.
Fertility Investigations and Assessment
A thorough assessment helps identify the cause and determine the best next steps.
Female Fertility Assessment
Ovulation tracking: menstrual history, blood tests (AMH, day-2 FSH/LH/oestrogen, progesterone, prolactin, thyroid functions)
Pelvic ultrasound: checks ovarian reserve (antral follicle count), uterus, endometrium, and detects conditions like fibroids or endometriosis
Tubal assessment (tubal dye study)
Cervical screening if due
Additional hormonal tests (thyroid, prolactin) if indicated
Male Fertility Assessment
Semen analysis to evaluate sperm count, motility, and morphology
Repeat testing may be recommended if the first sample is abnormal
In some cases, additional tests or referral to a male fertility specialist or urologist may be suggested
Surgical Procedures Used in Fertility Assessment and Management
Tubal Dye Study (HyCoSy, HSG or laparoscopy)
A procedure that uses dye and ultrasound (HyCoSy) or X-ray (HSG) to check whether the fallopian tubes are open.
Tubal dye study at the time of laparoscopy.
Helpful for diagnosing blockages or tubal damage.
Hysteroscopy
A small camera passed through the cervix to assess the uterine cavity.
Can diagnose and treat polyps, septum, submucosal fibroids, and scarring, which may affect implantation.
Often performed as a minor outpatient procedure.
Laparoscopy
Keyhole surgery to assess the pelvis, treat endometriosis, release adhesions, or remove fibroids affecting fertility.
Also used to confirm tubal patency by injecting dye during the procedure.
Offers both diagnosis and treatment in one operation.
These procedures can improve natural fertility and optimise outcomes before assisted reproduction.
When Referral to a Fertility Specialist Is Recommended
You may benefit from referral to a fertility specialist if:
You have been trying to conceive for 12 months (or 6 months if >35 years)
There are known factors such as endometriosis, PCOS, fibroids, or tubal blockage
Semen analysis is abnormal
Your AMH is low or cycles are very irregular
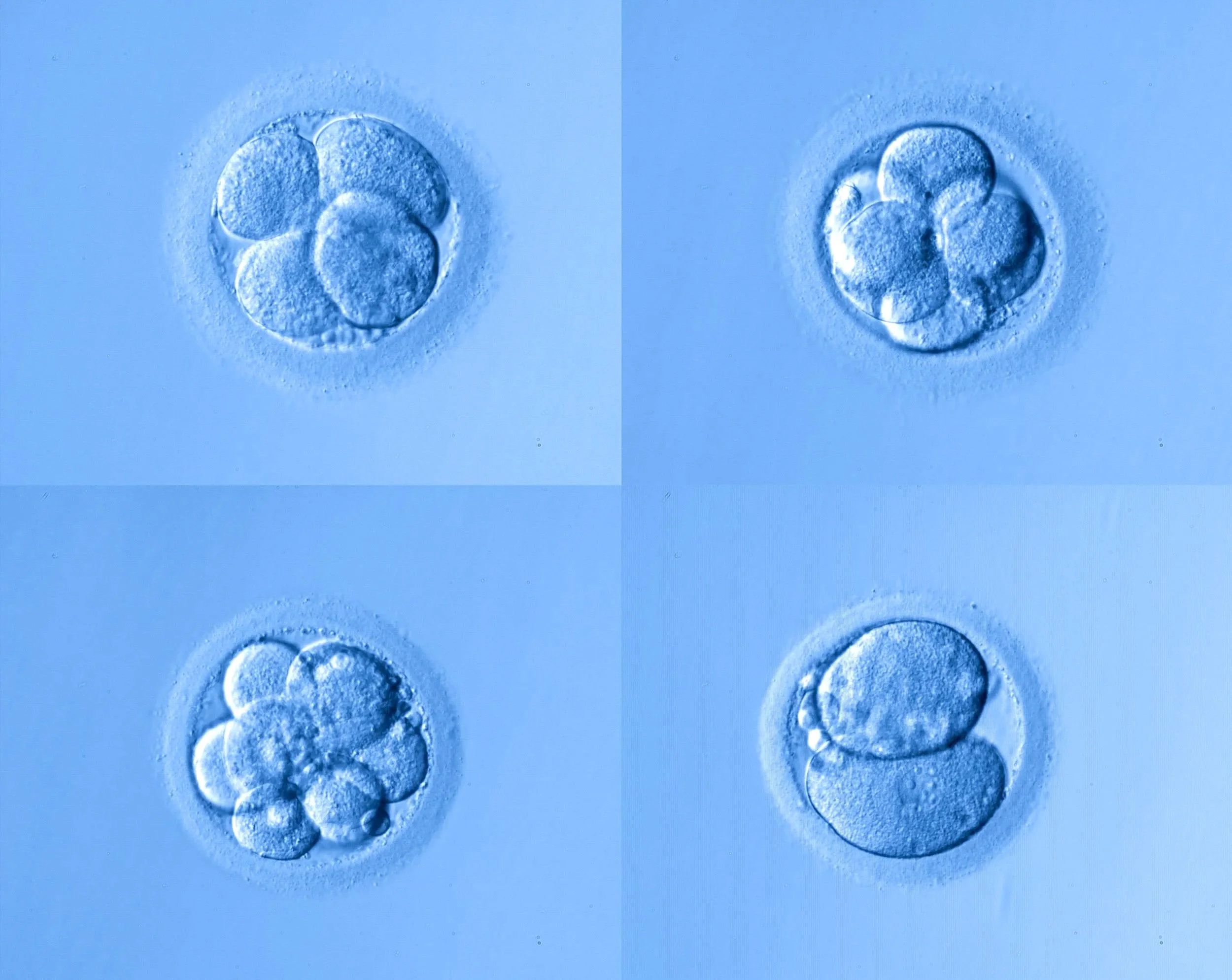
You require assisted reproductive technology (IUI, IVF, or ICSI)
Fertility specialists offer advanced care within a multidisciplinary team, including reproductive endocrinologists, andrologists, nurses, embryologists, counsellors, and genetic specialists.
How We Can Help
We provide comprehensive initial fertility assessment, including detailed history-taking, blood tests, pelvic ultrasound, tubal studies, and semen analysis coordination. We can also investigate and manage underlying gynaecological conditions affecting fertility, such as endometriosis and fibroids.
Anna has additional surgical training in advanced laparoscopic (keyhole) gynaecological surgery, allowing her to offer minimally invasive procedures - including laparoscopy for endometriosis, laparoscopic myomectomy, and hysteroscopy - to improve fertility outcomes with shorter recovery times, less pain, and smaller scars.
When needed, we work closely with fertility specialists to ensure timely referral and coordinated multidisciplinary care, supporting you through each step of your fertility journey.
